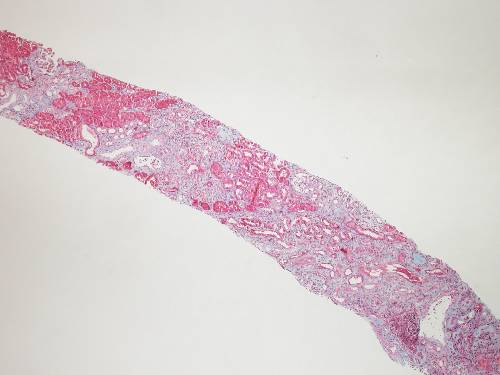
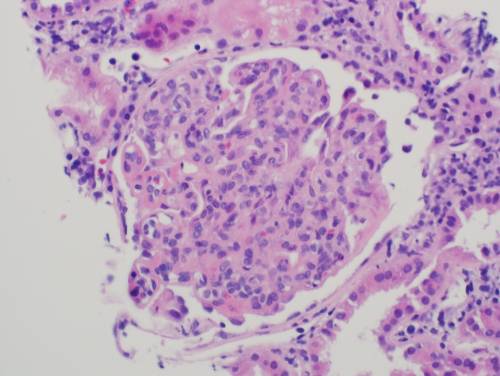
A 25 year-old male comes to the physician complaining of flank pain and hematuria. He says the pain is constant and dull. There is no frequency, urgency or dysuria. He has a history of mental retardation and seizures. On physical exam his blood pressure is 140/90 mm Hg, and his pulse is 80 bpm. He has multiple yellow papules across his nose and cheeks and numerous areas of blanched skin spots on his face. A 2-3 cm hypopigmented macule is noted on the right arm. CT scan of the head was done as patient presented with seizures. CT head was reported normal. CT scan of the abdomen shows bilateral hypodense fat containing renal masses and cysts.
What is the MOST likely diagnosis associated with these findings?
| A. Von Hippel Lindau | |
| B. Sturge Weber Syndrome | |
|
|
C. Tuberous Sclerosis |
| D. Osler Weber Rendu | |
| E. Neurofibromatosis type 2 |
 Omitted Omitted
|
Copyright © ABIM Exam World
Created On: 09/13/2017
Last Modified: 12/30/2017